fundsforNGOs - Grants and Resources for Sustainability
Grants and Resources for Sustainability

An Example Sample Project Proposal on “Healthcare Waste Management”
Healthcare waste management is a critical issue that needs immediate attention due to its potential impact on public health and the environment. This project proposal outlines a comprehensive plan for implementing effective healthcare waste management practices to mitigate risks associated with improper waste disposal in healthcare facilities. The primary goal is to establish a sustainable waste management system that ensures the safe handling, segregation, storage, transportation, and disposal of healthcare waste.
Project Objectives:
- Develop and implement a healthcare waste management policy in compliance with local regulations and international best practices.
- Raise awareness among healthcare workers, administrators, and support staff about the importance of proper waste management and their roles in implementing the system.
- Improve waste segregation practices to facilitate the proper handling and disposal of different categories of healthcare waste.
- Establish an efficient waste collection and transportation system to minimize the risk of contamination and promote safe waste disposal.
- Implement appropriate waste treatment and disposal methods, prioritizing environmentally friendly and sustainable options.
- Monitor and evaluate the effectiveness of the healthcare waste management system, identifying areas for improvement and implementing corrective measures as necessary.
Project Scope: This project will focus on healthcare facilities, including hospitals, clinics, laboratories, and other healthcare settings, within the target area. The scope encompasses all stages of waste management, from waste generation to final disposal. It will involve collaboration with key stakeholders, including healthcare facility administrators, waste management authorities, environmental agencies, and local communities.
Methodology:
The project will follow a phased approach to healthcare waste management implementation:
Over 25,000 NGOs, companies, and individuals have unlocked exclusive grants, resources, and opportunities with our Premium Membership – and now, it’s your turn! Take advantage of our biggest discount yet and start achieving your goals today. 💼✨ Don’t miss this chance to join the thriving community that’s already benefiting from Premium. Upgrade now at 78% off!
- Conduct a thorough assessment of the existing healthcare waste management practices and identify gaps and areas for improvement.
- Develop a comprehensive waste management policy and guidelines, tailored to the specific needs of the healthcare facilities.
- Create an implementation plan, including timelines, responsibilities, and resource requirements.
- Conduct training sessions and workshops to educate healthcare workers, administrators, and support staff about proper waste management practices.
- Provide training on waste segregation, handling, and storage techniques, emphasizing infection control and safety measures.
- Establish monitoring and reporting mechanisms to track compliance and identify training needs.
- Identify and procure necessary infrastructure and equipment for waste collection, segregation, storage, and transportation.
- Install appropriate waste disposal units, such as incinerators, autoclaves, or alternative treatment technologies, based on environmental suitability and cost-effectiveness.
- Ensure compliance with safety and environmental regulations during infrastructure setup.
- Implement the waste management system across healthcare facilities, ensuring proper segregation, storage, and transportation of waste.
- Conduct regular monitoring and audits to assess compliance with waste management policies and guidelines.
- Analyze waste management data to identify trends, patterns, and areas requiring improvement.
- Evaluate the effectiveness of the healthcare waste management system through periodic assessments and feedback from stakeholders.
- Implement corrective actions and improvements based on the evaluation findings.
- Share best practices and lessons learned to promote knowledge exchange and continuous improvement.
Expected Outcomes:
- Improved healthcare waste management practices in compliance with local regulations and international standards.
- Enhanced awareness and knowledge among healthcare workers, leading to increased compliance with waste management protocols.
- Reduction in healthcare-associated infections and environmental pollution resulting from improper waste disposal.
- Enhanced safety and protection for healthcare workers, patients, and the general public.
- Efficient utilization of resources and cost savings through optimized waste management practices.
Project Timeline: The project is anticipated to be implemented over a period of [insert duration], with specific milestones and deliverables outlined in the detailed project plan.
Budget: A detailed budget for the project, including expenses for infrastructure setup, equipment procurement, training sessions, monitoring activities, and evaluation processes, will be prepared during the planning phase.
Conclusion : The proposed healthcare waste management project aims to address the critical issue of improper waste disposal in healthcare facilities. By implementing effective waste management practices, we can significantly reduce the risks associated with healthcare waste and contribute to a healthier environment. We seek support and collaboration from relevant stakeholders to ensure the successful implementation of this vital project and its long-term sustainability. Together, we can make a positive impact on public health and the environment.
Next >> << Previous

Funds for NGOs Funds for Companies Funds for Media Funds for Individuals Sample Proposals
Contact us Submit a Grant Advertise, Guest Posting & Backlinks Fight Fraud against NGOs About us
Terms of Use Third-Party Links & Ads Disclaimers Copyright Policy General Privacy Policy
Premium Sign in Premium Sign up Premium Customer Support Premium Terms of Service

Healthcare Waste Management for Hospitals in Resource-Constrained Settings: What Determines Effective Implementation?
Add to collection, downloadable content.
- January 19, 2022
- Affiliation: Gillings School of Global Public Health, Department of Health Policy and Management
- The effective management of healthcare waste is a critical component of a hospital’s infection control program and is central to occupational safety for healthcare workers and the health of the environment and community. In low-income countries, where hospital administrators are burdened by resource constraints and struggle to maintain basic health services, healthcare waste management (HCWM) can be a significant challenge. There are, however, examples of hospitals in low-income countries that are effectively implementing HCWM systems that use new technology and practices and focus on reducing, reusing and recycling their waste. This research aimed to identify the determinants of effective implementation of the HCWM systems in three such hospitals located in Kathmandu, Nepal. This study utilized a multiple case study design with a mixed methods approach. A conceptual model for implementation effectiveness of complex innovations in organizational settings was used to guide the study design. The key findings from this study identified four determinants that facilitated effective implementation across all sites including 1) the presence of an innovation champion within the hospital who advocated for use of the system; 2) a strong perception of the primary users (nurses and ward attendants) that use of the system contributed to fulfillment of their group values such as doing no harm to patients and service to the community; 3) a partnership with a technical organization; and 4) strong implementation policies and practices. The study identified one determinant that acted as a barrier to effective implementation across all sites; hospital staff perceived that it was difficult for hospital visitors to comply fully with policies that required visitors to segregate all waste at source. There were differences in motivation to adopt and implement HCWM systems depending on the type of hospital (private, public, non-profit). The length of implementation and management engagement were also found to influence the level of implementation effectiveness. The findings suggest that large hospitals in low-income countries like Nepal can effectively manage their waste through systems that minimize harm to the environment, hospital staff and surrounding communities. The study provides recommendations for the type of support and inputs needed for effective implementation.
- August 2015
- medical waste
- healthcare waste management
- infection control
- implementation science
- hospital management
- Health services administration
- Environmental health
- Public health
- https://doi.org/10.17615/3jwb-bh64
- McPherson_unc_0153D_15671.pdf
- Dissertation
- In Copyright
- Babich, Suzanne
- Rutala, William
- Weiner, Bryan
- Robinson, Janet
- Doctor of Public Health
- University of North Carolina at Chapel Hill Graduate School
- Chapel Hill, NC
- There are no restrictions to this item.
- January 21, 2016
This work has no parents.
Select type of work
Master's papers.
Deposit your masters paper, project or other capstone work. Theses will be sent to the CDR automatically via ProQuest and do not need to be deposited.
Scholarly Articles and Book Chapters
Deposit a peer-reviewed article or book chapter. If you would like to deposit a poster, presentation, conference paper or white paper, use the “Scholarly Works” deposit form.
Undergraduate Honors Theses
Deposit your senior honors thesis.
Scholarly Journal, Newsletter or Book
Deposit a complete issue of a scholarly journal, newsletter or book. If you would like to deposit an article or book chapter, use the “Scholarly Articles and Book Chapters” deposit option.
Deposit your dataset. Datasets may be associated with an article or deposited separately.
Deposit your 3D objects, audio, images or video.
Poster, Presentation, Protocol or Paper
Deposit scholarly works such as posters, presentations, research protocols, conference papers or white papers. If you would like to deposit a peer-reviewed article or book chapter, use the “Scholarly Articles and Book Chapters” deposit option.
An official website of the United States government
Official websites use .gov A .gov website belongs to an official government organization in the United States.
Secure .gov websites use HTTPS A lock ( Lock Locked padlock icon ) or https:// means you've safely connected to the .gov website. Share sensitive information only on official, secure websites.
- Publications
- Account settings
- Advanced Search
- Journal List
Health Care Waste Management Improvement Interventions Specifications and Results: A Systematic Review and Meta-Analysis
Ali ashtari, jafar sadegh tabrizi, ramin rezapour, mohammad rashidian maleki, saber azami-aghdash.
- Author information
- Article notes
- Copyright and License information
Corresponding Author: Email: [email protected]
Received 2020 Jan 11; Accepted 2020 Mar 12.
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International license ( https://creativecommons.org/licenses/by-nc/4.0/ ). Non-commercial uses of the work are permitted, provided the original work is properly cited.
Background:
Given the importance of proper management of Health Care Waste Management (HCWM), comprehensive information on interventions in this field is necessary. Therefore, we aimed to systematically review and meta-analysis of characteristics and results of interventions in the field of HCWM.
The required data were gathered through searching the keywords such as waste management, biomedical waste, hospitals waste, health care waste, infectious waste, medical waste, Waste Disposal Facilities, Garbage, Waste Disposal Facilities, Hazardous Waste Sites in PubMed, Scopus, EMBASE, Google scholar, Cochrane library, Science Direct, web of knowledge, SID and MagIran and hand searching in journals, reference by reference, and search in Gray literatures between 2000 and 2019. CMA software: 2 (Comprehensive Meta-Analysis) was used to perform the meta-analysis.
Twenty-seven interventions were evaluated. Most of the studies were conducted after 2010, in the form of pre and post study, without control group, and in hospital. Interventions were divided into two categories: educational interventions (19 studies) and multifaceted managerial interventions (8 studies). The most studied outcome (in 11 studies) was KAP (knowledge, attitude and practice). The mean standard difference of interventions on KAP was estimated 3.04 (2.54–3.54) which was significant statistically ( P <0.05). Also, interventions were considerably effective in improving the indicators of waste production amount, waste management costs and overall waste management performance.
Conclusion:
Despite positive effect of interventions, due to the methodological deficiencies of published studies and high heterogeneity in results of studies, caution should be exercised in interpreting and using the results of the studies.
Keywords: Health care waste management, Systematic review, Meta-analysis, Critical analysis, Interventions
Introduction
The increasing health care needs of people in different countries have led to increase in the number of hospitals, clinics, laboratories, health centers, clinics, dental clinics and other health centers, which in turn has increased the amount and variety of medical waste ( 1 – 3 ). In addition to performing their duties, which include treating patients, providing health services, promoting sanitary and public health, health centers produce health waste that is itself a serious health and environmental problem ( 4 , 5 ). These types of wastes, due to its toxic and pathogenic risk factors, including pathological, pharmaceutical, chemical and radioactive substances, as one of the major pollutants of the environment and hazardous waste, is highly regarded ( 6 , 7 ). Since these wastes are highly contaminated with pathogens, exposure to humans can lead to dangerous infectious diseases ( 8 ). There is strong evidences that risk factors such as human immunodeficiency virus (HIV), hepatitis B and hepatitis C can also be transmitted through health system waste, with hospital waste play a key role in the pathogenesis and transmission of infection and environmental pollution ( 9 , 10 ).
Therefore, proper of Health Care Waste Management (HCWM), can prevent the spread of serious diseases that threaten the health of society and the environment and also prevent wasting of energy and costs ( 11 , 12 ). In recent years, many interventions and studies have been conducted in different countries to improve the performance of HCWM ( 16 – 13 ). Based on the searches, it appears that no study has been published that has systematically summarized the features and results of these interventions and critically evaluated them. Having reliable information about the results of interventions and programs implemented in the field of HCWM is essential for effective and scientific future planning and policy making. This requires reviewing the results and information of previous studies in this field and analyzing their quality. On the other hand, given these interventions have been designed and implemented in different ways and have had different results, systematically review of the characteristics and outcomes of these interventions can be useful in designing and implementing more effective interventions.
Therefore, we aimed to systematically review and meta-analysis of characteristics and results of interventions in the field of HCWM and critical analysis of their implementation.
Materials and Methods
This study was a systematic review and meta-analysis study, designed and conducted in 2019 in Tabriz University of Medical Science (TUOMS), using the systematic review approach taken from the book “Systematic Review to Support Evidence-Based Medicine” ( 17 ). Also it was in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyzes (PRISMA) ( 18 ).
Search strategy
The required data were gathered through searching the keywords such as waste management, biomedical waste, hospitals waste, health care waste, infectious waste, medical waste, Waste Disposal Facilities, Garbage, Waste Disposal Facilities, Hazardous Waste Sites and their Persian equivalents in PubMed, Scopus, EMBASE, Google scholar, Cochrane library, Science Direct, web of knowledge, SID and MagIran. The timeframe selected for searching the articles was 2000 to 2019. To identify and cover most of the published articles, after searching the databases, a number of high ranking journals were searched manually. After excluding articles that had little relevance to the objectives of the study and including the main articles, the references of the included articles was also searched to increase the confidence of identifying and reviewing existing articles. The databases of the European Association for Gray Literature Exploitation (EAGLE) and the Health Care Management Information Consortium (HMIC) were also searched for Gray literature.
Inclusion and exclusion criteria
Inclusion and exclusion criteria based on PICO model are presented in Table 1 .
Inclusion and exclusion criteria based on PICO model
Assessing Reporting Quality of Studies
The reporting quality of articles assessed by two members of the research team independently and using the checklists of pre and post studies (without control group), developed by the National Heart, Lung, and Blood Institute (NHLBI). This checklist contains 12 questions which have five options including “Yes”, “NO”, “Not reported”, “Cannot determine” and “Not applicable” ( 19 ). The articles were divided into three categories: good (score above 60), average (score between 40 and 59), and poor (score below 40). As one of the objectives of the present study was to critically evaluate the quality of interventions, no articles were excluded because of poor quality. Also, 6 articles that were conducted as the quality improvement projects, and did not fit well with the checklist questions, were not evaluated. In order to score questions on each checklist, the final agreement of the two evaluators was used as the decision criteria. If disagreement, the case was referred to third person with more knowledge and information in this field.

Data extraction
To extract the data, the extraction table was first designed manually through Word Microsoft 2010. Initially, the data of 3 papers were extracted experimentally through this form and problems in the original form were reformed. Data were extracted from the included articles by two individuals independently. Extracted data in article specification form included: author and year of publication, country of study, study design, study setting, and aim of study, participants and number, type of intervention, description of intervention implementation, main measured outcome and overall results. Endnote X5 reference manager software was used to organize the references.
Data Analysis Methods
Meta-analysis statistical methods were used to calculate the effect of interventions on knowledge, attitude and performance of employees. CMA software: 2 (Comprehensive Meta-Analysis) was used to perform the meta-analysis. Forest plot diagrams were used to report the results, where the size of each square represents the sample size and the lines on each side of the square represent 95% confidence interval for each study. Q and I 2 were used to assess the heterogeneity of the studies’ result. In this study, I 2 higher than 50%, identified as the criteria of articles’ heterogeneity. Random effects model was used, given the high heterogeneity of the study. Funnel Plot was also used to measure publication bias. To assess the statistical significance of the effects of interventions on knowledge, attitude and performance of employees, paired t test was used in SPSS (Chicago, IL, USA) software version 16. Other extracted data were analyzed using descriptive statistics (percentage, frequency, mean, etc.) and reported.
Ethical approval
This study was part of an approved study in the Research Ethics Committee of Tabriz University of Medical Science (ethical code: IR.TBZMED.REC.1398.1169).
Out of the 926 articles found from databases and other sources, 369 duplicate references were removed. In the title and abstract screening, 547 articles were removed. In the full text screening phase, 38 studies were excluded and finally 27 articles were included in the study ( Fig. 1 ).
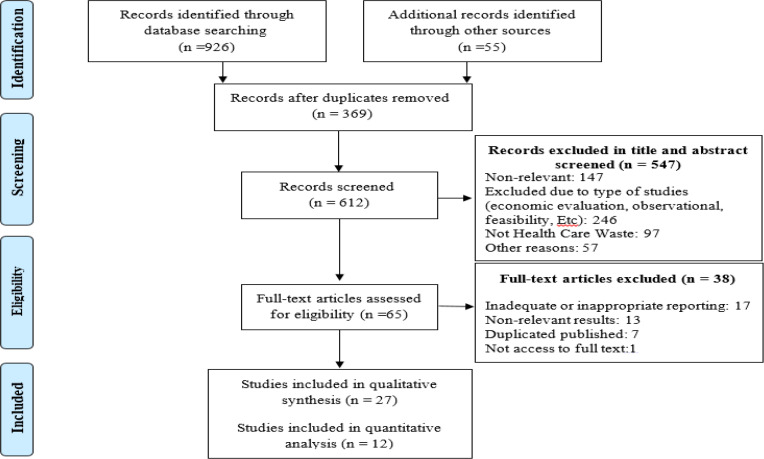
Searches and inclusion process
Time trend of publication
The time trend of publication of articles indicates that most studies (except one) were published after 2010 and meanwhile the most of them (6 studies) were published in 2017
Country of Studies
Published studies were conducted in 11 countries. Most studies were in India (10 studies), Pakistan (3 studies), Egypt (3 studies), Iran (2 studies) and the USA (2 studies). According to the latest world bank classification in 2019–2020, one study was conducted in a low-income country, 19 in lower-middle income countries, 3 in upper- middle-income countries and 4 in high-income countries.
Studies’ design
From 27 reviewed articles, 14 studies were performed in the form of before and after study without control group. Seven studies were quasi-experimental. Six studies were also included as quality improvement projects (1 clinical audit study, 3 six sigma studies, one TQM study and 1 quality improvement study). None of the studies were clinical trial.
Studies’ setting
Most studies (24 studies) were performed in the hospital. Two studies were conducted in primary health care centers and one study in a dental school clinic.
Studies’ participants
In 8 studies (1156 participants) the type of participants was not specified (generally written Health Care Workers), in two studies the hospital was studied unit. Other information about the different groups of participants is shown in Table 2 .
Information of different groups of participants in interventional studies to improve the health waste management
Studies in which participants are not identified separately.
Kind of interventions
Based on the interventions performed in the included studies, the interventions were divided into two categories of educational interventions including 19 studies and multifaceted managerial interventions including 8 studies. The educational interventions were implemented mostly in the form of lectures, booklets, discussions, posters and practical examples. In addition to providing training, multifaceted management interventions focused more on changing waste management policies and processes, developing standards and guidelines, and providing the equipment and facilities required to better waste management.
Measured outcomes
The most studied outcomes (in 11 studies) were the knowledge, attitude, and performance (KAP) ( Fig. 2 ).
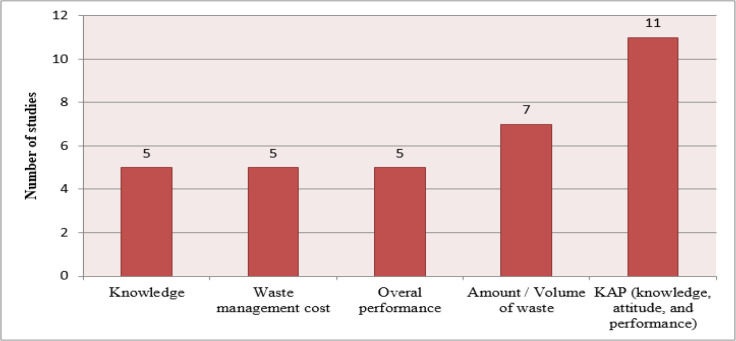
Measured Outcomes of Included Interventional Studies to Improve Health care Waste Management
Results of Interventions
KAP: Based on the results of the interventions, the estimated standard difference in mean of the interventions effect, generally on KAP, was 3.04 [2.54–3.54]. Meanwhile the heterogeneity of the intervention results was high [Q = 885 df = 21 P <0.001 I2 = 97.6]. This was estimated 3.12 [2.54–3.70] at knowledge, 2.74 [1.05–4.43] at attitude and 2.87 [1.68–4.06] at performance ( Fig. 3 ). The results of evaluating the likelihood of publication bias also indicated a relatively low likelihood of publication bias ( Fig. 4 ). The results of statistical analysis also showed interventions significantly improve the knowledge, attitude and performance of staff ( P <0.05).
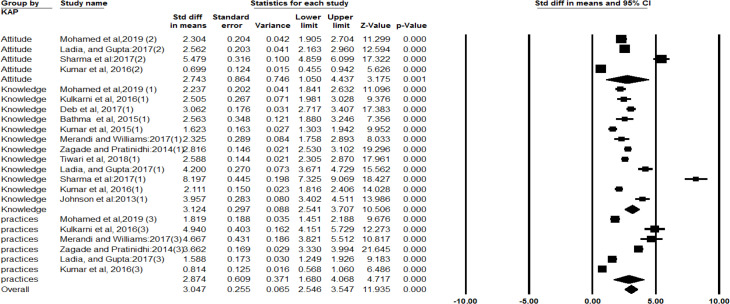
Results of meta-analysis of the interventions’ impact on knowledge, attitude and practice of health care providers based on random effects model
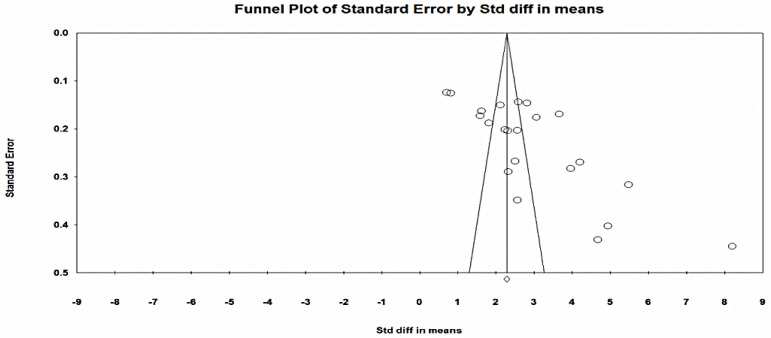
Funnel plot to evaluate the probability of publication bias in the results of interventions to improve health care waste management
The measured outcomes in other studies also was knowledge, attitude, and performance of service providers, but were not able to enter the meta-analysis, however, their results also indicate a significant improvement in the knowledge, attitude and performance of health care providers.
Impact of interventions on amount of waste, waste management costs and overall waste management performance
The results of the studies indicate that, like providers’ knowledge, attitude and performance, interventions also improve the indicators of produced waste amount, waste management costs and overall waste management performance, significantly ( Table 3 ).
Results of Reporting Quality Assessment
Among 21 articles that their reporting quality was assessed, 10 articles were high-quality, 7 were low-quality, and 4 were medium-quality. The major weakness of the articles was that they did not repeat the assessments several times before and after the intervention.
The results of the review of the publication time showed that most of the studies (except one) were published after 2010. This indicates a significant researchers’ delay in recognizing the importance of improving the status health waste management. Because the issue of HCWM is not a new issue, and the health waste generation has been raised simultaneously with the activity of health organizations. Hence it needs that with more attention to this issue, backwardness in this area be compensated. Because delays in this regard will have very undesirable consequences for health care organizations themselves, health care providers and the whole community ( 30 , 31 ).
Most of the studies were conducted in middle- and low-income countries. Considering the time trend of publication of articles, one of the possible reasons could be that many years ago (not included in the study timeframe) health care organizations in High-Income Countries (HICs) solved the problems of HCWM and Low and Middle Income Countries (LMICs) recently have realized the importance of this issue. So that, attention to the rules and regulations of waste management in health care organizations is unprecedented and has been paid attention to in recent years ( 13 ). However, there are many differences and shortcomings in this regard. Therefore, it seems that applying the experiences of successful countries in this field and adapting them to the local context of organizations in LMICs, is helpful. Use of the most up-to-date recommendations, guidelines and waste management promotion models can also be helpful ( 32 – 36 ).
Most of the included studied were in the hospital setting, and only 2 studies were conducted in primary health centers. One of the possible reasons for this may be the importance, the volume and the hazardous degree of produced waste in hospitals. Because of the nature of the care provided in hospitals, both the volume of waste is high and due to its toxic and pathogenic risk factors, including pathological, pharmaceutical and chemical and radioactive substances is known as one of the major pollutants of the environment ( 30 , 37 , 38 ). However, waste management in primary health care for many reasons, such as the large number of centers, more relevance with the community and people, the provision of a wide range of care, and most importantly the low attention by researchers and authorities to waste management in this sector, it is also very important ( 39 – 41 ). The results of review the literature and experiences of countries also show that in different countries as well this issue has been neglected and few studies have been done in this field ( 42 – 44 ). Therefore, more attention needs to be paid to these centers by both authorities and researchers.
Reviewing the type of interventions showed that most of the interventions were educational (19 studies), while a limited number of studies (8 studies) were multi-faceted managerial interventions. Although the results of educational interventions showed that these interventions were effective, it is important to note that in most educational interventions the outcomes are KAP which seem to be relatively easier to influence on these variables, and on the other hand, the impact of improving these variables on overall waste management improvement without regard to other variables and requirements, is negligible. Thus, the results of the meta-analysis of the impact of interventions on providers’ KAP showed that the greatest improvement occurred in awareness and the attitude and performance that could be more influential than awareness were less improved than awareness. While, the variables studied in multifaceted managerial interventions are mostly the produced waste volume, costs reduction and the overall waste management performance improvement, and these consequences directly and significantly improve waste management. Therefore, it is recommended in the future studies to pay more attention to multifaceted managerial interventions in addition to educational interventions.
The results of the present study showed that the interventions significantly reduced the costs of produced waste. Although waste costs account for a significant percentage of the costs of health care systems, these organizations usually do not pay much attention to these costs, and there are usually no accurate cost accounting and analysis systems in this field ( 45 – 47 ). The approximate annual cost of waste management in health systems is € US5,079,191, or € US2.36 kg-1, and direct costs of waste production and other related costs could be reduced through improving the segregation system and getting tax for extra waste production ( 48 ). Therefore, it is recommended that managers and authorities to plan to reduce the costs of waste production ( 49 , 50 ), trough using recommended methods such as costing and costs reduction.
Although based on the evaluation checklist, the reporting quality of articles was relatively good, but the quality of interventions had many limitations and drawbacks, some of the most important are briefly mentioned here. The first issue is the quality of the interventions (especially educational interventions). Because educational interventions were mostly lecture, and they were limited in terms of number and time of interventions, had many flaws. Another important issue was how to measure the impact of interventions, as in most studies participants’ KAP had only been assessed once before and after the intervention. While it is recommended that the impact of interventions be measured several times over time to assess the sustainability of the interventions, this has been the case in only a few limited studies. In terms of costing, the types of costs (direct and indirect) were also not specified. The next issue is the studies’ design, most of them were before and after study without control group and few studies were quasi-experimental (controlled). Randomization was rarely had considered in the selection of participants. Also, in many studies interventions were not described clearly and completely. Therefore, it is recommended that scholars be more careful in designing and performing interventions, use available guidelines in this area to conduct more appropriate intervention with more robust methodology, and editors and reviewers of journals be also more careful in publishing articles.
Although based on our best knowledge, the present study is the first study to systematically and comprehensively review interventions in HCWM, however there are some limitations to the present study. One of the most important of these limitations is that searches were limited to Farsi and English, because it was not possible for researchers to search for and evaluate articles published in other languages. Also, due to methodological deficiencies in included studies, and the high heterogeneity in their results, it is not possible for researchers to conclude with high reliability.
Interventions to improve HCWM indicators including KAP of service providers, produced waste amount, waste management costs and overall waste management performance were effective significantly, however, because of the methodological deficiencies in published studies and high heterogeneity over the results, caution should be exercised in interpreting and using the results of studies. Also, it is recommended that future studies use more of multifaceted managerial interventions, pay more attention to primary health care centers, and design and implement interventions with stronger and more reliable methodologies with control groups.
Ethical considerations
Ethical issues (Including plagiarism, informed consent, misconduct, data fabrication and/or falsification, double publication and/or submission, redundancy, etc.) have been completely observed by the authors.
Acknowledgements
This study was funded by School of Management and Medical Informatics, Tabriz University of Medical Science, Tabriz, Iran. This school has supported this study as a Master’s thesis under the MSc Training Program
Conflict of interest
The authors declare that there is no conflict of interest.
- 1. Windfeld ES, Brooks MS. (2015). Medical waste management - A review, J Environ Manage. 163:98–108. [ DOI ] [ PubMed ] [ Google Scholar ]
- 2. Eker HH, Bilgili MS, Sekman E, et al. (2010). Evaluation of the regulation changes in medical waste management in Turkey. Waste Manag Res, 28(11):1034–8. [ DOI ] [ PubMed ] [ Google Scholar ]
- 3. Al-Momani H, Obaidat M, Khazaleh A, et al. (2019). Review of medical waste management in Jordanian health care organisations. Br J Healthc Manag, 25(8):1–8. [ Google Scholar ]
- 4. Eren E, Tuzkaya UR. (2019). Occupational health and safety-oriented medical waste management: A case study of Istanbul. Waste Manag Res, 37(9):876–884. [ DOI ] [ PubMed ] [ Google Scholar ]
- 5. Gao Q, Shi Y, Mo D, et al. (2018). Medical waste management in three areas of rural China. PLoS One, 13(7):e0200889. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 6. Olaniyi FC, Ogola JS, Tshitangano TG. (2019). Efficiency of Health Care Risk Waste Management in Rural Healthcare Facilities of South Africa: An Assessment of Selected Facilities in Vhembe District, Limpopo Province. Int J Environ Res Public Health, 16(12):2199. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 7. Acharya A, Gokhale VA, Joshi D. (2014). Impact of biomedical waste on city environment: Case study of Pune, India. J Appl Chem,6(6):21–7. [ Google Scholar ]
- 8. Bdour A, Altrabsheh B, Hadadin N, et al. (2007). Assessment of medical wastes management practice: a case study of the northern part of Jordan. Waste Manag, 27(6):746–59. [ DOI ] [ PubMed ] [ Google Scholar ]
- 9. Chaerul M, Tanaka M, Shekdar AV. (2008). A system dynamics approach for hospital waste management. Waste Manag, 28(2):442–9. [ DOI ] [ PubMed ] [ Google Scholar ]
- 10. Yizengaw E, Getahun T, Geta M, et al. (2018). Sero-prevalence of hepatitis B virus infection and associated factors among health care workers and medical waste handlers in primary hospitals of North-west Ethiopia. BMC Res Notes, 11(1):437. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 11. Babanyara Y, Ibrahim D, Garba T, et al. (2013). Poor Medical Waste Management (MWM) practices and its risks to human health and the environment: a literature review. Int J Environ Ealth Sci Eng, 11(7):1–8. [ Google Scholar ]
- 12. Mastorakis NE, Bulucea CA, Oprea TA, et al. (2010). Environmental and health risks associated with biomedical waste management. Develop Energy Environ Economics, 2010:287–94. [ Google Scholar ]
- 13. Ali M, Wang W, Chaudhry N, et al. (2017). Hospital waste management in developing countries: A mini review. Waste Manag Res, 35(6):581–92. [ DOI ] [ PubMed ] [ Google Scholar ]
- 14. Bai VR, Vanitha G, Zainal Ariff AR. (2013). Effective hospital waste classification to overcome occupational health issues and reduce waste disposal cost. Infect Control Hosp Epidemiol, 34(11):1234–1235. [ DOI ] [ PubMed ] [ Google Scholar ]
- 15. Kwikiriza S, Stewart AG, Mutahunga B, et al. (2019).A Whole Systems Approach to Hospital Waste Management in Rural Uganda. Front Public Health,7:136. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 16. Motta O, Zarrella I, Cucciniello R, et al. (2018). A new strategy to control the proliferation of microorganisms in solid hospital waste and the diffusion of nosocomial infections. Infez Med,26(3):210–215. [ PubMed ] [ Google Scholar ]
- 17. S Khan K, Kunz R, Kleijnen J, et al. Systematic reviews to support evidence-based medicine Mazurek Melnyk B, editor 2011. [ Google Scholar ]
- 18. Moher D, Liberati A, Tetzlaff J, et al. (2009). Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med, 6(7):e1000097. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 19. National Heart Lung and Blood Institute Quality Assessment Tool for Before-After (Pre-Post) Studies With No Control Group [National Heart Lung and Blood Institute web site] 2019. [Accessed october 23].
- 20. Askarian M, Heidarpoor P, Assadian O. (2010). A total quality management approach to healthcare waste management in Namazi Hospital, Iran. Waste Manag, 30(11):2321–6. [ DOI ] [ PubMed ] [ Google Scholar ]
- 21. Martin DM, Yanez N, Treggiari MM. (2017). An initiative to optimize waste streams in the operating room: Recycling in the operating room (RECOR) project. AANA J, 85(2):108–12. [ PubMed ] [ Google Scholar ]
- 22. Mokuolu O, Akindele R, Olawumi H. (2016). Development of improved solid hospital waste management practices in a Nigerian Tertiary Hospital. Nigerian J Technol, 35(3):674. [ Google Scholar ]
- 23. Mosquera M, Andrés-Prado MJ, Rodríguez-Caravaca G, et al. (2014). Evaluation of an education and training intervention to reduce health care waste in a tertiary hospital in Spain. Am J Infect Control, 42(8):894–7. [ DOI ] [ PubMed ] [ Google Scholar ]
- 24. Perrego K. (2017).Improving Staff Knowledge of Perioperative Regulated-Waste Management. AORN J, 105(1):85–91. [ DOI ] [ PubMed ] [ Google Scholar ]
- 25. Johnson KM, González ML, Dueñas L, et al. (2013). Improving waste segregation while reducing costs in a tertiary-care hospital in a lower–middle-income country in Central America. Waste Manag Res, 31(7):733–8. [ DOI ] [ PubMed ] [ Google Scholar ]
- 26. Aboelnour A, Abuelela MH. (2019). Increase adherence to waste management policy at healthcare facility in Egypt. Bulletin of the National Research Centre, 43(1):29. [ Google Scholar ]
- 27. Tabrizi JS, Saadati M, Heydari M, et al. (2018). Medical waste management improvement in community health centers: an interventional study in Iran. Prim Health Care Res Dev, 20:1–6. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 28. Stonemetz J, Pham JC, Necochea AJ, et al. (2011). Reduction of regulated medical waste using lean sigma results in financial gains for hospital. Anesthesiol Clin, 29(1):145–52. [ DOI ] [ PubMed ] [ Google Scholar ]
- 29. Almuneef M, Memish ZA. (2003). Effective medical waste management: it can be done. Am J Infect Control, 31(3):188–92. [ DOI ] [ PubMed ] [ Google Scholar ]
- 30. Gielar A, Helios-Rybicka E. (2013). Enviromental impact of a hospital waste incineration plant in Krakow (Poland). Waste Manag Res, 31(7):722–8. [ DOI ] [ PubMed ] [ Google Scholar ]
- 31. Rao PH. (2008).Report: Hospital waste management--awareness and practices: a study of three states in India. Waste Manag Res, 26(3):297–303. [ DOI ] [ PubMed ] [ Google Scholar ]
- 32. Eleyan D, Al-Khatib IA, Garfield J. (2013). System dynamics model for hospital waste characterization and generation in developing countries. Waste Manag Res, 31(10):986–95. [ DOI ] [ PubMed ] [ Google Scholar ]
- 33. Townend WK, Cheeseman CR. (2005). Guidelines for the evaluation and assessment of the sustainable use of resources and of wastes management at healthcare facilities. Waste Manag Res, 23(5):398–408. [ DOI ] [ PubMed ] [ Google Scholar ]
- 34. Kühling J-G, Pieper U. (2012). Management of healthcare waste: developments in Southeast Asia in the twenty-first century. Waste Manag Res, 30:100–4. [ DOI ] [ PubMed ] [ Google Scholar ]
- 35. Ho CC, Liao CJ. (2011). The use of failure mode and effects analysis to construct an effective disposal and prevention mechanism for infectious hospital waste. Waste Manag, 31(12):2631–7. [ DOI ] [ PubMed ] [ Google Scholar ]
- 36. Reza Sabour M, Mohamedifard A, Kamalan H. (2007). A mathematical model to predict the composition and generation of hospital wastes in Iran. Waste Manag, 27(4):584–7. [ DOI ] [ PubMed ] [ Google Scholar ]
- 37. Tsakona M, Anagnostopoulou E, Gidarakos E. (2007). Hospital waste management and toxicity evaluation: A case study. Waste Manag, 27(7):912–20. [ DOI ] [ PubMed ] [ Google Scholar ]
- 38. Nemathaga F, Maringa S, Chimuka L. (2008). Hospital solid waste management practices in Limpopo Province, South Africa: A case study of two hospitals. Waste Manag, 28(7):1236–45. [ DOI ] [ PubMed ] [ Google Scholar ]
- 39. Alves SB, e Souza ACS, Tipple AFV, et al. (2014). The reality of waste management in primary health care units in Brazil. Waste Manag Res. 32:40–7. [ DOI ] [ PubMed ] [ Google Scholar ]
- 40. Saadati M, Azami-Aghdash S, Rezapour R. (2020). Medical Waste Management in Community Health Centers: Different Experience From East Azerbaijan Province, Iran. Int Q Community Health Educ, 40(2):159–60. [ DOI ] [ PubMed ] [ Google Scholar ]
- 41. Tabrizi JS, Rezapour R, Saadati M, et al. (2018). Medical waste management in community health centers. Iran J Public Health, 47(2):286–291. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 42. Win E, Saw Y, Oo K, et al. (2019). Healthcare waste management at primary health centres in Mon State, Myanmar: The comparisons between hospital and non-hospital type primary health centres. Nagoya J Med Sci, 81:81–91. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 43. Sadeghi H, Fazlzadeh M, Hazrati S, et al. (2012). Survey of waste management practices at health centers of Ardebil City. J Health, 2(4):17–27. [ Google Scholar ]
- 44. Organization WH (2005). Management of solid health-care waste at primary health-care centres: A decision-making guide.
- 45. Himmelstein DU, Woolhandler S, Wolfe SM. (2004). Administrative waste in the US health care system in 2003: the cost to the nation, the states, and the District of Columbia, with state-specific estimates of potential savings. Int J Health Serv, 34(1):79–86. [ DOI ] [ PubMed ] [ Google Scholar ]
- 46. Rashidian A, Alinia C, Majdzadeh R. (2015). Cost-effectiveness analysis of health care waste treatment facilities in iran hospitals; a provider perspective. Iran J Public Health, 44(3):352–60. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 47. Lee BK, Ellenbecker MJ, Moure-Ersaso R. (2004). Alternatives for treatment and disposal cost reduction of regulated medical wastes. Waste Manag, 24(2):143–51. [ DOI ] [ PubMed ] [ Google Scholar ]
- 48. Vaccari M, Tudor T, Perteghella A. (2018). Costs associated with the management of waste from healthcare facilities: An analysis at national and site level. Waste Manag Res, 36(1):39–47. [ DOI ] [ PubMed ] [ Google Scholar ]
- 49. Soares SR, Finotti AR, Prudêncio da Silva V, et al. (2013). Applications of life cycle assessment and cost analysis in health care waste management. Waste Manag, 33(1):175–83. [ DOI ] [ PubMed ] [ Google Scholar ]
- 50. D’Souza BC, Seetharam AM, Chandrasekaran V, et al. (2017). Comparative analysis of cost of biomedical waste management across varying bed strengths in rural India. Int J Healthc Manag, 11(1):1–6. [ Google Scholar ]
- View on publisher site
- PDF (1.1 MB)
- Collections
Similar articles
Cited by other articles, links to ncbi databases.
- Download .nbib .nbib
- Format: AMA APA MLA NLM
Add to Collections

IMAGES
COMMENTS
Dec 21, 2021 · Result Results showed that 61.2% of the surveyed clinics had poor healthcare waste management practices, out of which, 56.8% had poor waste segregation practice, 55.0% had poor waste collection ...
medical waste management was harmed by a lack of funding, insufficient logistics, a lack of disposal sites, and a lack of understanding. This demonstrated a 74.6 percent variance in
Healthcare waste management is a critical issue that needs immediate attention due to its potential impact on public health and the environment. This project proposal outlines a comprehensive plan for implementing effective healthcare waste management practices to mitigate risks associated with improper waste disposal in healthcare facilities. The primary goal is to establish a sustainable
Feb 10, 2021 · This study examines the available knowledge and current practices in medical/ healthcare waste management worldwide, particularly in countries with transitional economies, including the dependence ...
Aug 31, 2023 · Gunawardana KD: An analysis of medical waste management practices in the health care sector in Colombo. MEQ. Jul. 2018;29(5):813–825. 10.1108/MEQ-02-2018-0032 [Google Scholar] 4. Zhao H, et al. : A review on emergency disposal and management of medical waste during the COVID-19 pandemic in China. Sci. Total Environ.
Jan 19, 2022 · Affiliation: Gillings School of Global Public Health, Department of Health Policy and Management; Abstract. The effective management of healthcare waste is a critical component of a hospital’s infection control program and is central to occupational safety for healthcare workers and the health of the environment and community.
Al-Momani H, Obaidat M, Khazaleh A, et al. (2019). Review of medical waste management in Jordanian health care organisations. Br J Healthc Manag, 25(8):1–8. [Google Scholar] 4. Eren E, Tuzkaya UR. (2019). Occupational health and safety-oriented medical waste management: A case study of Istanbul. Waste Manag Res, 37(9):876–884.
Aug 12, 2015 · Bio-medical waste management is critical for ensuring public health and environmental sustainability. However, due to the inherent ambiguities and complexities involved with waste characteristics ...
The problem of medical waste is a national, regional, and international problem. Medical waste management interventions are very important so that the waste generated is managed properly and correctly. This is because medical waste is included in the category of hazardous and toxic waste. Some medical waste is included in the
2.2 COMPONENT 2: NON-BURN WASTE TREATMENT TECHNOLOGY (Medical waste autoclave, autoclave housing and medical waste transport vehicle) Based on my TOR, this component has eight (8) major activities, namely: 1) comments on the technical proposals for the design and build of the non-burn waste treatment